Cognitive and behavioral health has become a rising imperative across health care, policy, and everyday life. As the wave of baby boomers surpasses age 65, the need for comprehensive support in managing cognitive decline and behavioral health issues has intensified.
Given this shift, it’s not surprising that regulators are increasing resources and incentives for early detection and management of conditions like dementia. The Centers for Medicare & Medicaid Services (CMS) now mandates cognitive impairment screenings during annual wellness visits and offers reimbursement for assessment—a clear signal that cognitive health is essential to sustainable patient care.
The challenge, however, remains significant. Projections estimate that by 2050, approximately 139 million people worldwide will have dementia (Alzheimer’s Disease International), and under current standards, nearly 60 percent of cases might go undetected (Lang et al., 2017), revealing a critical need for better screening tools and expanded coding to accurately capture the prevalence of this disease.
With the V28 model rolling out through 2026, health care providers face a pivotal opportunity in advancing dementia care. The updated risk adjustment model emphasizes accurate dementia coding, urging systems to rethink patient workflows, documentation, and billing practices to keep pace with growing demand. This article explores how V28 changes reshape cognitive care, offering practical steps for organizations to adapt to this evolving landscape.
Understanding the V28 shift and its impact on dementia diagnosis
The V28 model, fully replacing V24 by 2026, shifts coding to ICD-10-CM, expands HCC categories from 86 to 115, and refines risk adjustment for a more accurate reflection of patient health status. These changes support the CMS’s aim for a streamlined, equitable reimbursement system aligned with health care needs today.
Here are just a few of the projected benefits of the V28 model:
1. More accurate representation of patient health status and resource needs. Given that dementia, for example, is underdiagnosed, V28 is positioned to incentivize the accurate detection and diagnosis of the condition, aligned to its prevalence in the population. The new model, leveraging ICD-10-CM codes, aims to improve the precision of risk adjustment and payment calculations.
2. Clearer categorization and weighting of risk scores. Under V28, risk scores more accurately correlate with the actual health care costs incurred by different patient populations.
3. Fairer and more equitable payment distribution. More equitable distribution reduces the risk of over- or under-payments to Medicare Advantage plans.
4. Aligns coding and reimbursement for Medicare Advantage and Fee-For-Service Medicare. By standardizing these processes, CMS aims to create a more unified and transparent system that supports both quality care delivery and financial sustainability. This alignment is crucial in reducing discrepancies and improving the overall efficiency of the Medicare system.
These changes are part of CMS’ broader effort to modernize the risk adjustment framework, making it more reflective of today's health care landscape and ensuring that funds are allocated efficiently to support necessary patient care without incurring unnecessary costs.
A new era for dementia coding
With the transition to V28, some organizations worry about revenue impacts, assuming an even distribution of the impacted codes across patient populations. But V28 brings critical updates that, in particular, could be transformative for dementia care.
Notably, the model expands high-RAF dementia categories and continues to support reimbursement for substance use disorders and psychiatric conditions, preserving vital funding channels (CMS, Pinnacle).
While fewer diagnostic codes might suggest potential revenue dips, the emphasis on coding precision and high-RAF dementia expansion opens doors for more accurate risk adjustment. This shift aligns with industry goals for better data capture and cost prediction. Given the often-overlooked prevalence of dementia, providers now have a chance to close this gap, reach underdiagnosed groups, and secure the necessary funding to serve these populations effectively.
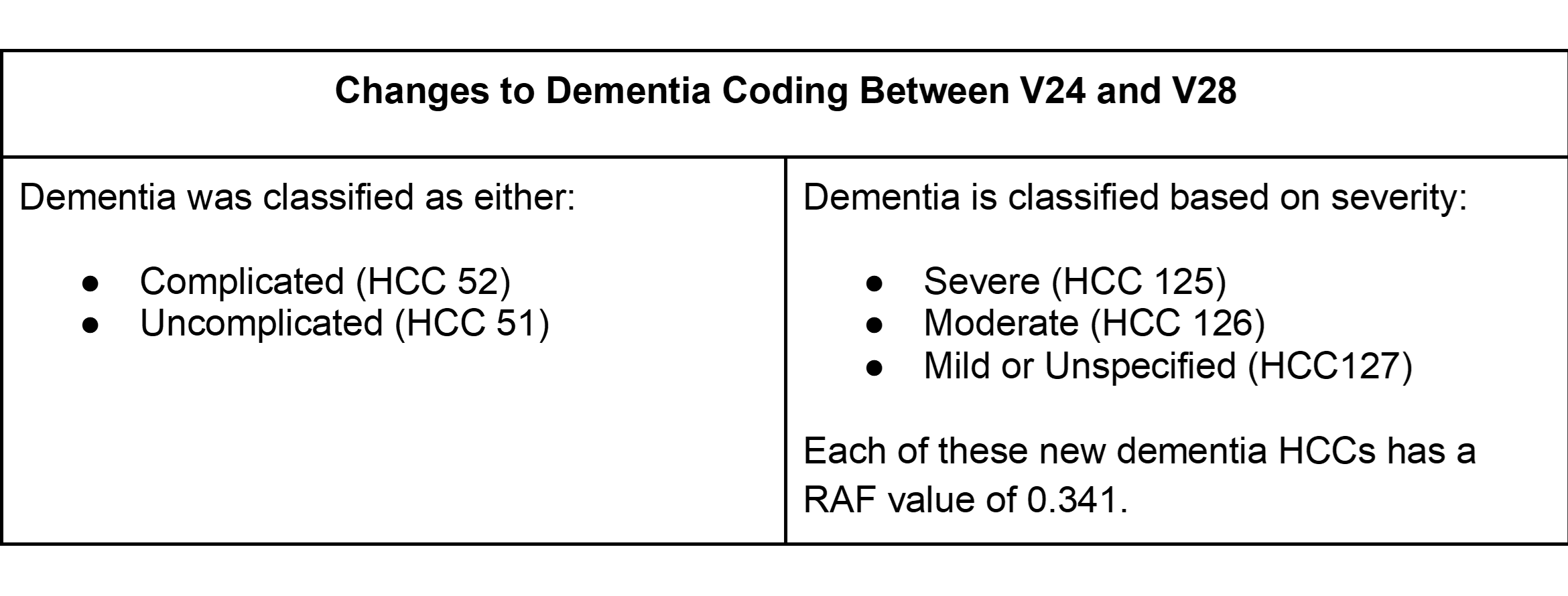
Previously, diagnosing early-stage dementia might have required multiple codes to capture various symptoms and stages. Now, with expanded categories under V28, providers can use a single, more comprehensive code to capture mild or moderate dementia stages. This streamlined approach allows for more accurate coding and can improve reimbursement by reflecting the true complexity of the patient’s condition.
Preparing for a successful transition to V28
As 2026 approaches, health systems will need to stay up to date with the regulatory changes and adjust to the adoption of V28 practices. Below, we outline a few key steps that will continue to be important in this transition.
1. Navigating dual HCC models
Organizations must manage both V24 and V28 HCC models until 2026. Health systems can ease this transition by identifying top HCCs for their population. For practices with many seniors, keeping both dementia codes on hand may streamline the shift to V28.
2. Prioritizing comprehensive documentation
Accurate risk adjustment hinges on precise documentation. Investing in digital tools that capture detailed cognitive insights and align with DSM-5 criteria will enable practices to categorize conditions accurately under the V28 model and avoid unnecessary regulatory scrutiny.
3. Using both models for RAF calculation
To navigate risk scoring in 2025, consider blending models: calculate RAF scores by combining 33 percent of V28 with 67 percent of V24 to gain a balanced assessment.
4. Enabling accurate, early detection
With the V28 model prioritizing dementia care, organizations should consider advanced digital tools that will enable earlier detection and diagnosis. Unlike traditional dementia screeners, which primarily detect more severe cases, online platforms with DSM-5-aligned assessments provide a more comprehensive view of cognitive, functional, and behavioral health, effectively identifying even mild impairments.
Advancing dementia care for greater growth
Changes to the V28 risk adjustment model mark a shift toward proactive dementia care, responding to the rising needs of an aging population. By staying informed on policy updates, adopting advanced screening tools, and making cognitive assessments routine, organizations can enhance patient outcomes while supporting sustainable business growth. This shift not only strengthens dementia detection but also aligns with a forward-thinking, value-based care model focused on achieving better patient outcomes.
About the author
Emily Montemayor, CCS, CMBCS, COC, CPC, CPMA, is a distinguished health care professional with over a decade of specialized expertise in revenue integrity, compliance, CDI, provider education, and auditing. As the medical coding support manager at Creyos and a recognized subject matter expert, she has been instrumental in driving optimized reimbursement strategies and reinforcing revenue integrity for our clients. Montemayor’s influence extends globally, where she has trained health care professionals and pioneered innovative coding solutions. Her thought leadership is showcased through published articles in AAPC magazines and impactful collaborations with MedLearn Media on book
editorials and educational webcasts. She is dedicated to advancing the health care industry through her commitment to education, compliance excellence, and innovative content development.
