When it comes to improving CAHPS® results, health plans often face a challenging paradox: How can you personalize care and support at an individual level while still managing it across millions of members? The answer is harnessing the power of advanced AI technology based on behavioral science principles. By diving into each member’s unique circumstances, MedOrion’s platform enables health plans to address personal health barriers at scale, which leads to better medication adherence, HEDIS®, and CAHPS outcomes, and stronger member relationships. Here’s why identifying these barriers is critical, how technology makes it achievable, and the impact on CAHPS scores.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA) and any reference thereto by RISE Health does not imply any endorsement by NCQA of RISE Health and its offerings.
Why we must address personal health barriers
Improving health outcomes isn’t just about offering the right services and sending generic reminders to members—it’s about understanding what motivates them and hinders them from making healthier choices. MedOrion’s technology pinpoints these barriers, moving beyond surface-level issues to address the real pain points members experience in their health care journeys.
In today’s health care landscape, this level of understanding isn’t just an advantage—it’s essential. As CAHPS surveys increasingly reflect member satisfaction, health plans can’t afford to overlook the specific needs and experiences of every member. MedOrion makes this possible by translating behavioral research into actionable insights that reveal the factors influencing each member’s decisions.
How MedOrion’s technology helps achieve this goal
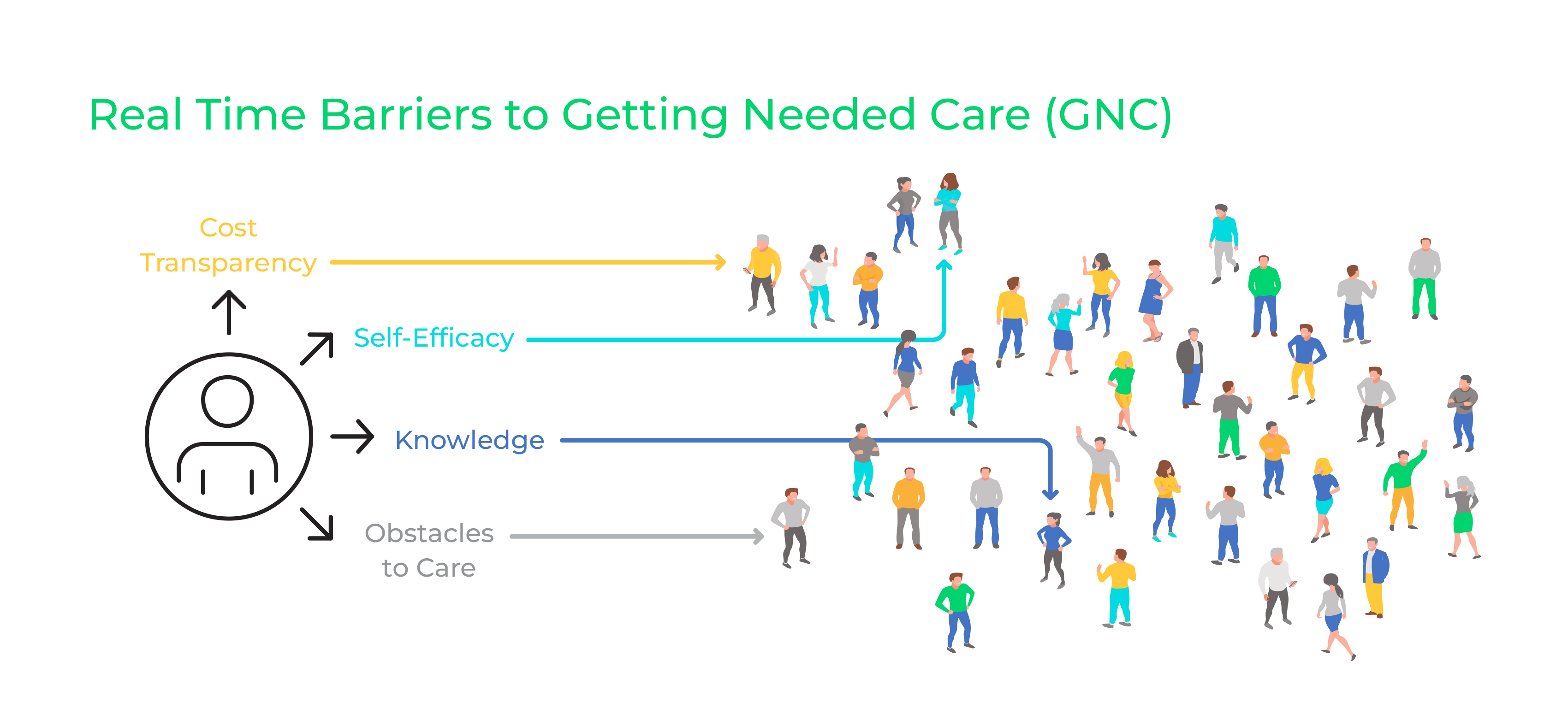
The science behind this approach takes us from assumptions to evidence-based actions. By associating specific behaviors with potential barriers, MedOrion’s technology uses behavioral science and AI to generate data-driven insights that paint a holistic picture of each member. Here’s how MedOrion breaks down personal barriers at scale:
● Data harmonization: The platform integrates diverse data sources, including claims, social determinants of health, demographics, and more, to create comprehensive electronic behavior records. This data harmonization allows MedOrion to pinpoint specific barriers unique to each member.
● Automated barrier identification: MedOrion’s solution automatically detects individual barriers in real-time, helping health plans prioritize their focus based on the most pressing needs. Instead of treating members as a collective, this approach allows for targeted actions reflecting each person’s challenges.
● Personalized engagement strategies: Once barriers are identified, the platform generates customized engagement strategies. These tailored communications and nudges are delivered across various channels, ensuring that members receive relevant information in a way that’s meaningful and accessible to them.
● Continuous improvement: To ensure the effectiveness of interventions, MedOrion measures impact by comparing outcomes against control groups. This ongoing refinement process ensures that strategies evolve, maintaining their effectiveness and supporting sustained improvements in CAHPS measures like “Getting Needed Care” and “Getting Appointments and Care Quickly.”
Impact on CAHPS scores and member experience
The results speak for themselves. MedOrion’s approach has led to a notable 5 percent increase in CAHPS GNC and a 26 percent reduction in complaint rates—a clear sign that understanding and addressing personal barriers translates into real-world outcomes. By resolving these underlying issues, MedOrion’s technology not only helps health plans improve their CAHPS scores but also builds stronger, trust-based relationships with members. Members feel heard, their needs are met, and they’re more likely to stay loyal to their health plans.
This approach offers a strategic advantage, allowing health plans to support their members more effectively and enhance their overall experience. In today’s competitive health care environment, addressing personal barriers at scale is not only possible but necessary for health plans aiming to improve Centers of Medicare & Medicaid Services’ Star rating outcomes. MedOrion’s technology helps health plans create a deeply personalized member experience, turning individual challenges into opportunities for positive change.
Interested in learning more about improving CAHPS results? Join our upcoming live webinar “Unlock New CAHPS Insights: Fireside Chat with Industry Experts” on Dec 4th at 11:00 AM EST. Save your seat right here.
